From Polio to Covid: The Tech That's Saving Lives
Polio Epidemic – Early 1900s
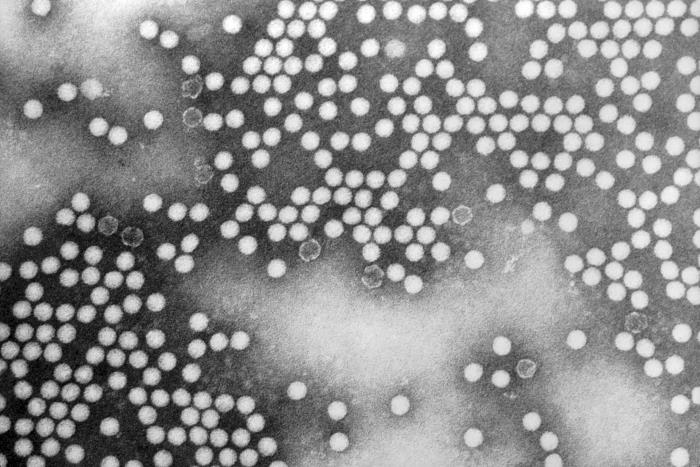
Polio is a virus that spreads through person-to-person contact and can infect a person’s spinal cord. Most people who get infected will not have visible symptoms, while others will present with flu-like symptoms. A smaller proportion of the population will develop more serious symptoms such as a feeling of pins and needles in their legs (paraesthesia), meningitis, or paralysis. It is this paralysis that often can lead to permanent disability and death because the virus affects the muscles that help the person breathe. Even after recovery, a small group of patients will experience post-polio syndrome.
Barbara Robin Smith, born in Dunedin in 1930, was diagnosed with polio at seven years old:
“I thought it was because I had eaten mashed parsnips, potatoes, and carrots, which I loathed as a child, and I threw up at midday dinner. My grandmother said, 'She has had too much sun.' I knew I must have been ill when the doctor came to the beach house from Dunedin to Brighton Beach because you never had the doctor come to the house. As this was the 1st of January 1937 and there was a very big epidemic of infantile paralysis, I guess my grandmother had suspicions that it wasn’t just too much sun."
"I don’t remember very much after that; I must have had a high temperature. The first things I remember afterwards, are coming conscious of plaster casts on my legs. I was totally paralysed except for my respiratory system, and it would have been months later that I remember that I was in bed with awful plaster casts that itched. The first time that I was taken downstairs and out onto the veranda as a treat. I also remember screaming, obviously as an adult, I realised that I had become so used to the bedroom that I had lost confidence in being taken away, a sort of cabin fever as it were.”
Polio in Aotearoa
Polio was only recognised sporadically before 1900 but spread rapidly throughout the western world during the first half of the 20th Century. Thousands died worldwide and many more were paralysed for life. New Zealand was not spared during this epidemic. An official report by the special committee investigating the safety of polio vaccines in 1983 recalled “Epidemic poliomyelitis was the most terrifying epidemic condition in the country and the professional and public fear was justified as no specific measure of control was known.”
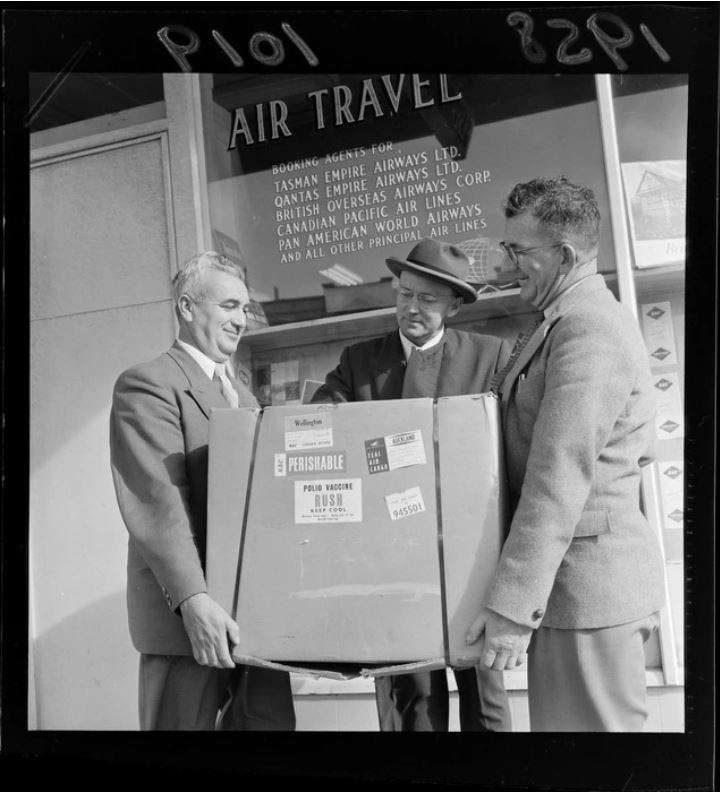
New Zealand’s first major recorded polio outbreak was in 1914 — it killed 25 people. Outbreaks occurred again in 1916, 1925, 1927, 1937, 1948–49, 1952–53, and 1955–56. Between 1915 and 1965 there were approximately 9,434 reported cases of polio; of these 790 deaths occurred. The worst year for deaths from polio was in 1925 when 173 people died. It wasn’t until the introduction of a polio vaccine in 1956 that polio outbreaks started to be controlled. The Ministry of Health says the last case of “wild” polio virus in New Zealand was in 1977. No cases of vaccine-associated paralytic poliomyelitis have occurred in New Zealand since the introduction of inactivated polio vaccine in 2002. To date, polio has been eradicated in every county in the world except for Nigeria, Pakistan, and Afghanistan.
Iron Lung Technology
The iron lung, also known as a tank respirator, was invented in 1927 at the Harvard School of Public Health by Phillip Drinker, assistant professor in the Department for Ventilation and Illumination, and Louis Agassiz Shaw Jr., instructor of physiology. The prototype iron lung was described as a huge metal box with a set of vacuum cleaners attached at one end to pump air in and out. The patient's whole body was enclosed in the airtight chamber except the head, which protruded from the box through a tight rubber seal to ensure air didn’t escape.

The purchase and shipping of iron lungs from the United States was so restrictive, and often unattainable during the depression of the 1930s, that many health departments in countries around the world turned to their own engineers to come up with cheaper alternatives. In New Zealand, Fred C. Jacobs, the chief engineer for the Auckland Hospital Board designed his version of the iron lung and had his son Bill Jacobs build it. Auckland Hospital Superintendent Dr J.F. Caughey and Dr J.W. Craven both consulted and supervised the project. It was built in the Auckland Hospital workshops around 1935–36 and is the first iron lung to have been used in New Zealand.
The use of the iron lung required the patient to be put on a stretcher inside the steel welded chamber with their head protruding out of the box through a hole in the door. Once the door has been secured, a variable-speed air pump was connected to the inside of the chamber and set in motion. This pump raises and lowers the pressure of the air causing the patient’s chest, and subsequently, their lungs, to be contracted and expanded so they can breathe.
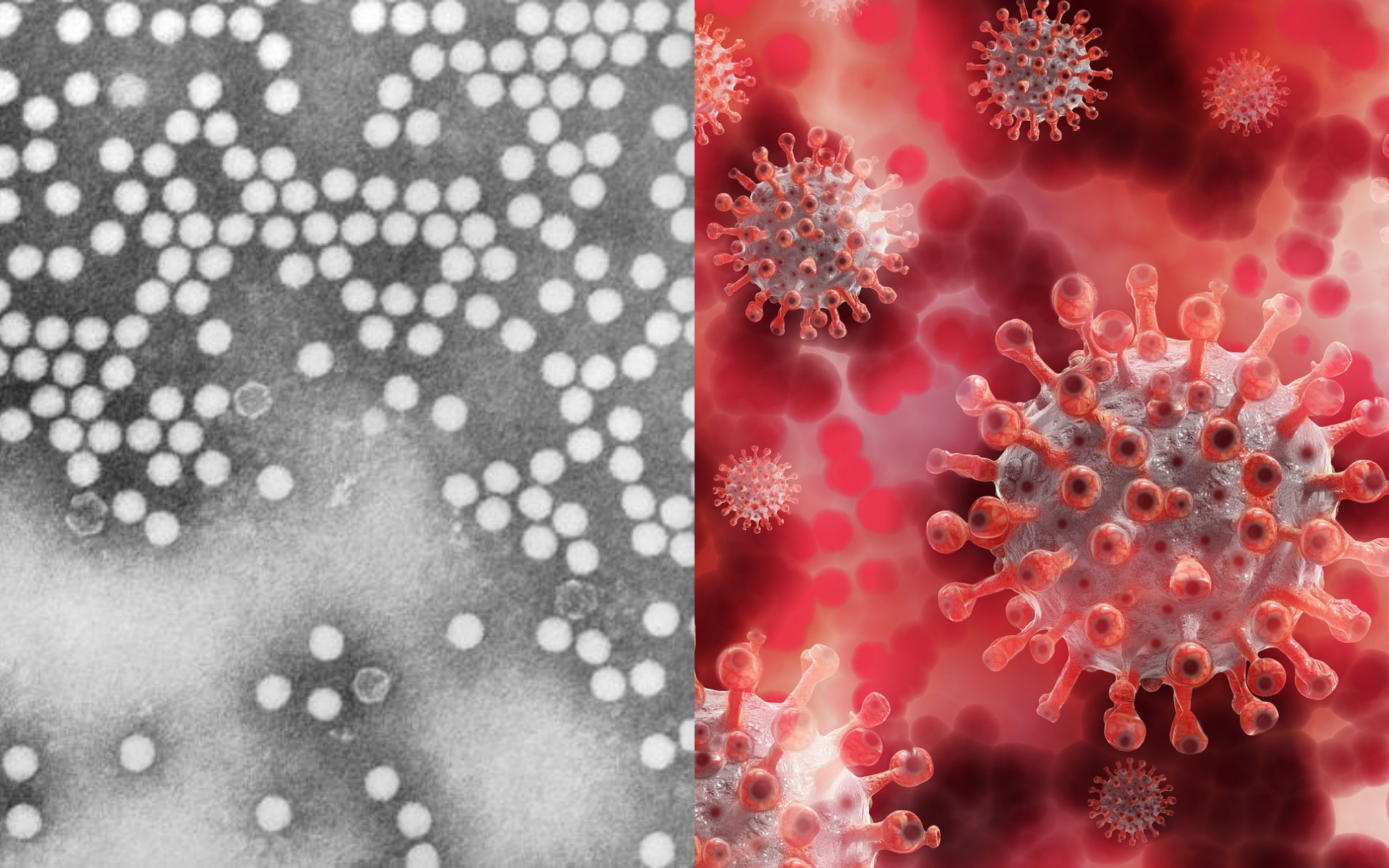
COVID-19 Pandemic – 2019
COVID-19 (SARS-CoV-2) was first discovered in Wuhan, China, and was declared a public health emergency of international concern on 30 January 2020 and was labelled as a pandemic on 11 March 2020.
SARS-CoV-2 stands for Severe Acute Respiratory Syndrome Coronavirus 2 and attacks the respiratory system of those infected by the virus. It is unknown where the virus originated from, though it does have zoonotic (animal to human) origins.
The most common symptoms include fever, cough, headache, fatigue, breathing difficulties, loss of taste and smell. There are several other less common symptoms and over one-third of cases are asymptomatic, meaning they may have no symptoms at all. This can make it harder to determine who is infectious, meaning transmission chains can grow undetected.
COVID-19 is transmitted from person to person via human droplets and airborne particles containing the virus. These are produced by breathing, coughing, sneezing, etc. A person can breathe these in, get sprayed by infected droplets, or via contaminated surfaces.
The incubation period before you present symptoms can be up to 14 days, and even if someone is not symptomatic, they can still pass on the virus. Testing locations were set up by governments worldwide, which include either a nasal swab or saliva test. This has been a key part of managing the transmission rate as it allows people to know when they test positive and to stay in self-isolation at home until their 14 days of infection is over.
Transmission and Health Response
Because we live in such a fast-paced world, slowing down a virus globally is tricky. Between international travel and daily commuters, people are moving around the world at a particularly faster pace than they did when the polio epidemic occurred all around the globe.
A combination of this fast-paced world, limited preventative care until the recent vaccine, and hostility towards lockdowns, means we have had approximately (as of this writing) 350 million cases of COVID-19 and 5.6 million deaths. COVID-19 hospitalisations have been high and taxing on our health care workers. Separate COVID-19 wards have been erected, ventilators that help people breathe when their lungs are full of infectious fluid have had to be rationed due to extreme demand, and there was a saying going around in the health care world, “Once you go on a vent(ilator), you’re not coming off.” Thousands of health care heroes have become infected and died from COVID-19 due to caring for record numbers of pandemic patients.
There have been reports of mass graves due to the sheer number of deaths that funeral companies and communities could just not manage. In the USA, there were cold trucks outside of funeral homes, meant for victims of COVID-19 as there was no room left inside to preserve their bodies for the family.
COVID-19 In Aotearoa
New Zealand has been lucky enough to scrape through the COVID-19 pandemic with a smaller number of cases compared to other countries. This does not mean that COVID-19 hasn’t impacted the people of Aotearoa massively. As of this writing, we have sadly lost 52 lives and have had 15,250 cases, a sad outcome for all those impacted and disadvantaged because of it.
Through several lengthy lockdowns, mask mandates, and social distancing, we have managed to stop the widespread transmission of COVID-19 in the Aotearoa community. MIQ (Managed Isolation and Quarantine) is used for international arrivals to stop border cases from entering the community. Through scientific guidance, the Government has introduced these isolation requirements to ensure the wider community is protected.

We have now seen three major variants of COVID-19 which have swept the world by storm. There is the original virus, the Delta variant, and the Omicron variant. The first two have sent Aotearoa into snap lockdowns for periods ranging between 6 weeks – 107 days. The Omicron variant recently reached our community and the entire country has shifted into Red Light Restrictions. Thankfully, Aotearoa is at 93% vaccination rate for those eligible, as of this writing.
Preventative Technology
While measures like hand washing and especially face masks can slow the spread of COVID-19, they can be less effective due to human error.
In terms of vaccines, several international pharmaceutical companies developed their own formula, all with varying minor side effects and immunity percentages. These vaccines have proven effective against all three variants of the virus. Aotearoa started the vaccine rollout in March 2021. Currently there are three doses recommended, the New Zealand Government recommends three weeks between the first two, and four months until your get your third "booster" vaccination.
The purpose of these vaccines is to reduce serious symptoms, hospitalisation and death, and to slow down the transmission rate between people. Clinical trials found the Pfizer vaccine offered 95% protection against the symptoms of COVID-19.
We hope to see an end to this pandemic soon – via new technologies like vaccines and antiviral medicines, while trusting that fact-based science is key to us all making it out safely.
Story by Christen McAlpine, Registrar, and Makayla Wallace-Tidd, Communications Coordinator, MOTAT
Links:
MOTAT COVID-19 Collection
Items and audio recordings that are a part of our Covid-19 collection, which aims to document this time via the innovations created in New Zealand since March 2020.
Citation:
McAlpine, Christen, and Wallace-Tidd, Makayla. From Polio to Covid: The Tech That's Saving Lives. MOTAT Museum of Transport and Technology. First published: 26 January
2022. URL: https://www.motat.nz/collections-and-stories/stories/from-polio-to-covid-the-tech-thats-saving-lives